- Gemcitabine is indicated for the treatment of locally advanced or metastatic bladder cancer in combination with cisplatin.
- Gemcitabine is indicated for the treatment of patients with locally advanced or metastatic adenocarcinoma of the pancreas.
- Gemcitabine, in combination with cisplatin, is indicated as first-line treatment for patients with locally advanced or metastatic non-small cell lung cancer (NSCLC). Gemcitabine monotherapy may be considered in elderly patients or those with a performance status of 2.
- Gemcitabine is indicated for the treatment of patients with locally advanced or metastatic epithelial ovarian carcinoma, in combination with carboplatin, in those with relapsed disease following a recurrence-free interval of at least six months after platinum-based first-line therapy.
- Gemcitabine, in combination with paclitaxel, is indicated for the treatment of patients with unresectable, locally recurrent, or metastatic breast cancer who have relapsed following adjuvant or neoadjuvant chemotherapy. Prior chemotherapy should have included an anthracycline, unless clinically contraindicated.
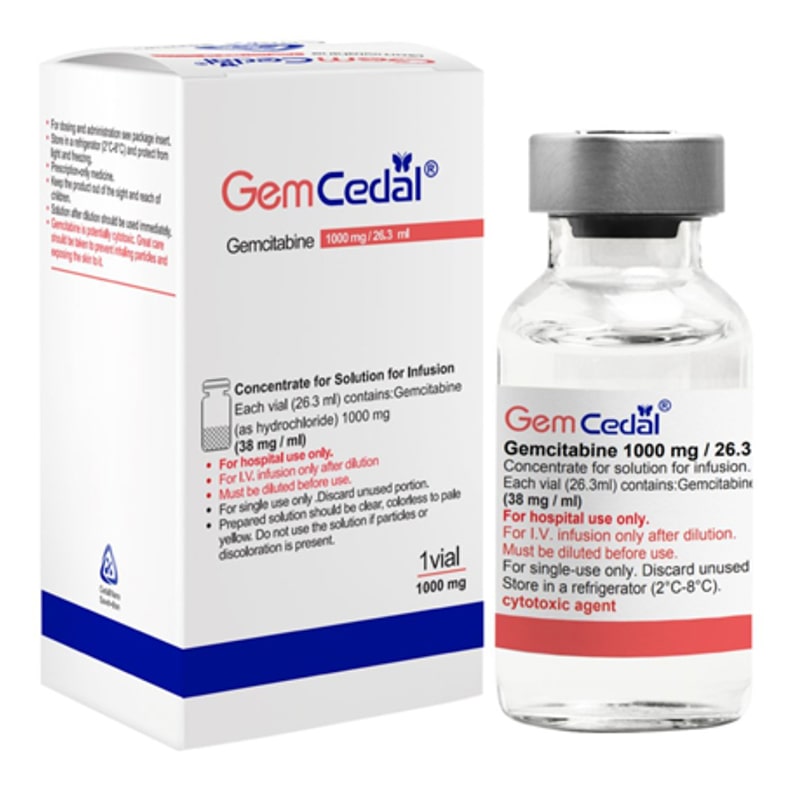
GemCedal®
Generic Name
Brand Name
Drug Class
Dosage Form
Indications
Contradications
Warnings and Precautions
Dosage and Administration
Adverse Reactions
Drug Interactions
Use in pregnancy and lactation
Storage Conditions
Indications
Contradications
- Hypersensitivity to the active substance or to any of the excipients listed in section 9.
- Breast-feeding
Warnings and Precautions
Prolongation of the infusion time and increased dosing frequency have been shown to increase toxicity.
Hematological toxicity
Gemcitabine can suppress bone marrow function, as manifested by leucopenia, thrombocytopenia, and anemia.
Patients receiving gemcitabine should be monitored prior to each dose for platelet, leukocyte, and granulocyte counts. Suspension or modification of therapy should be considered when drug-induced bone marrow depression is detected. However, myelosuppression is typically short-lived and usually does not result in dose reduction, and rarely necessitates discontinuation.
Peripheral blood counts may continue to decline even after gemcitabine administration has been discontinued. In patients with impaired bone marrow function, treatment should be initiated with caution. As with other cytotoxic treatments, the risk of cumulative bone marrow suppression must be considered when gemcitabine is administered in combination with other chemotherapeutic agents.
Skin and subcutaneous tissue disorders
Severe cutaneous adverse reactions (SCARs), including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and acute generalized exanthematous pustulosis (AGEP), which can be life-threatening or fatal, have been reported in association with gemcitabine treatment. Patients should be informed of the signs and symptoms and monitored closely for skin reactions. If signs or symptoms suggestive of these conditions appear, gemcitabine should be discontinued immediately.
Hepatic and renal impairment
Gemcitabine should be used with caution in patients with hepatic impairment or impaired renal function, as there is insufficient information from clinical studies to provide clear dose recommendations for this patient population.
Administration of gemcitabine in patients with concurrent liver metastases or a medical history of hepatitis, alcoholism, or liver cirrhosis may lead to worsening of underlying hepatic impairment.
Laboratory evaluation of renal and hepatic function (including virological tests) should be performed periodically.
Concomitant radiotherapy
Concomitant radiotherapy (given together or ≤7 days apart): Toxicity has been reported.
Live vaccinations
Yellow fever vaccine and other live attenuated vaccines are not recommended in patients treated with Gemcitabine.
Nervous system
Posterior Reversible Encephalopathy Syndrome (PRES)
Cases of posterior reversible encephalopathy syndrome (PRES) with potentially severe consequences have been reported in patients receiving gemcitabine, either as monotherapy or in combination with other chemotherapeutic agents.
Most gemcitabine-treated patients who developed PRES experienced acute hypertension and seizures, although other symptoms such as headache, lethargy, confusion, and visual disturbances including blindness have also been reported.
Diagnosis is optimally confirmed by magnetic resonance imaging (MRI). PRES is typically reversible with appropriate supportive care.
If PRES occurs during gemcitabine therapy, the drug should be permanently discontinued, and supportive measures—including blood pressure control and anti-seizure treatment—should be promptly implemented.
Cardiovascular
Due to the risk of cardiac and/or vascular disorders with gemcitabine, particular caution must be exercised with patients presenting a history of cardiovascular events.
Capillary leak syndrome
Capillary leak syndrome has been reported in patients receiving gemcitabine, either as monotherapy or in combination with other chemotherapeutic agents. The condition is generally treatable if recognized early and managed appropriately; however, fatal cases have been reported.
This syndrome involves systemic capillary hyperpermeability, in which fluid and proteins leak from the intravascular space into the interstitial compartment. Clinical features include generalized edema, weight gain, hypoalbuminemia, severe hypotension, acute renal impairment, and pulmonary edema.
If capillary leak syndrome develops during gemcitabine therapy, treatment should be discontinued and supportive care initiated. Notably, capillary leak syndrome may occur in later cycles of therapy and has been associated in the literature with adult respiratory distress syndrome (ARDS).
Pulmonary
Pulmonary effects, sometimes severe—such as pulmonary edema, interstitial pneumonitis, or adult respiratory distress syndrome (ARDS)—have been reported in association with gemcitabine therapy. The exact etiology of these effects remains unknown.
If such effects occur, discontinuation of gemcitabine should be considered. Early initiation of supportive care measures may help to improve or stabilize the condition.
Renal
Haemolytic Uraemic Syndrome (HUS)
Clinical findings consistent with haemolytic uraemic syndrome (HUS) have been rarely reported (based on post-marketing data) in patients receiving gemcitabine. HUS is a potentially life-threatening condition.
Gemcitabine should be discontinued at the first signs suggestive of microangiopathic hemolytic anemia, such as a rapid decline in hemoglobin accompanied by thrombocytopenia, or elevations in serum bilirubin, creatinine, blood urea nitrogen (BUN), or lactate dehydrogenase (LDH).
Renal failure associated with HUS may not be reversible upon discontinuation of therapy, and dialysis may be required.
Dosage and Administration
Gemcitabine should only be prescribed by a physician qualified in the use of anti-cancer chemotherapy.
Dosage
Bladder cancer
Combination use
The recommended dose for gemcitabine is 1000 mg/m2, given by 30-minute infusion. The dose should be given on Days 1,8 and 15 of each 28-day cycle in combination with cisplatin. Cisplatin is given at a recommended dose of 70 mg/m2 on Day1 following gemcitabine or day 2 of each 28-day cycle. This 4-week cycle is then repeated. Dosage reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient.
Pancreatic cancer
The recommended dose of gemcitabine is 1000 mg/m2, given by 30-minute intravenous infusion. This should be repeated once weekly for up to 7 weeks followed by a week of rest. Subsequent cycles should consist of injections once weekly for 3 consecutive weeks out of every 4 weeks. Dosage reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient.
Non small Cell lung cancer
Monotherapy
The recommended dose of gemcitabine is 1000 mg/m2, given by 30-minute intravenous infusion. This should be repeated once weekly for 3 weeks, followed by a 1-week rest period. This 4-week cycle is then repeated. Dosage reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient.
Combination use
The recommended dose for gemcitabine is 1250 mg/m2 body surface area given as a 30-minute intravenous infusion on Day 1 and 8 of the treatment cycle (21 days). Dosage reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient. Cisplatin has been used at doses between 75-100 mg/m2 once every 3 weeks.
Breast cancer
Combination use
Gemcitabine in combination with paclitaxel is recommended using paclitaxel (175 mg/m2) administered on Day 1 over approximately 3-hours as an intravenous infusion, followed by gemcitabine (1250 mg/m2) as a 30-minute intravenous infusion on Days 1 and 8 of each 21-day cycle. Dose reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient. Patients should have an absolute granulocyte count of at least 1,500 (x106/l) prior to initiation of gemcitabine + paclitaxel combination.
Ovarian cancer
Combination use
Gemcitabine in combination with carboplatin is recommended using gemcitabine 1000 mg/m2 administered on Days 1 and 8 of each 21-day cycle as a 30-minute intravenous infusion. After gemcitabine, carboplatin will be given on Day 1 consistent with a target Area under curve (AUC) of 4.0 mg/ml·min. Dosage reduction with each cycle or within a cycle may be applied based upon the grade of toxicity experienced by the patient.
Method of administration
Gemcedal® is tolerated well during infusion and may be administered ambulant. If extravasation occurs, generally the infusion must be stopped immediately and started again in another blood vessel. The patient should be monitored carefully after the administration.
Instructions for dilution
An approved diluent for Gemcedal® solution is sodium chloride 9 mg/ml (0.9%) solution for injection (without preservative).
- Use the aseptic technique during any dilution of Gemcedal® for intravenous infusion administration.
- Parenteral medicinal products should be inspected visually for particulate matter and discolouration prior to administration. If particulate matter is observed, do not administer.
- Any unused medicinal product or waste material should be disposed of in accordance with local requirements
Adverse Reactions
Like all medicines, Gemcedal® can cause side effects, although not everybody gets them.
The most common side effects are hair loss and a reduced number of blood cells. After the end of treatment your hair should grow again and your blood count should return to normal.
>10%:
- Cardiovascular: Peripheral edema (20%), edema (13%)
- Central nervous system: Drowsiness (11%)
- Dermatologic: Skin rash (30%), alopecia (15%)
- Gastrointestinal: Nausea and vomiting (69%), diarrhea (19%), stomatitis (11%) Genitourinary: Proteinuria (45%), hematuria (35%)
- Hematologic & oncologic: Anemia (68%; grade 3: 7%; grade 4: 1%), neutropenia (63%; grade 3: 19%; grade 4: 6%), thrombocytopenia (24%; grade 3: 4%; grade 4: 1%), hemor- rhage (17%; grade 3: <1%; grade 4: <1%)
- Hepatic: Increased serum ALT (68%; grade 3: 8%, grade 4: 2%), increased serum AST (67%; grade 3: 6%; grade 4: 2%), increased serum alkaline phosphatase (55%; grade 3: 7%; grade 4: 2%), increased serum bilirubin (13%; grade 3: 2%, grade 4: <1%) Infection: Infection (16%)
- Renal: Increased blood urea nitrogen (16%)
- Respiratory: Dyspnea (23%; grade 3: 3%; grade 4: <1%), flu-like symptoms (19%) Miscellaneous: Fever (41%)
1% to 10%:
- Central nervous system: Paresthesia (10%; grade 3: <1%)
- Local: Injection site reaction (4%)
- Renal: Increased serum creatinine (8%)
- Respiratory: Bronchospasm (<2%)
<1%
postmarketing, and/or case reports (reported with single-agent use or with combination therapy): Adult respiratory distress syndrome, anaphylactoid reaction, anorexia, arthralgia, bullous skin disease, capillary leak syndrome, cardiac arrhythmia, cardiac failure, cellulitis, cerebrovascular accident, constipation, desquamation, digital vasculitis, gangrene of skin or other tissue, hemolytic-uremic syndrome, hepatic failure, hepatic sinusoidal obstruction syndrome (formerly known as hepatic veno-occlusive disease), hepatotoxicity (rare), hyperglycemia, hypertension, hypocalcemia, hypotension, increased gamma-glutamyl transferase, interstitial pneumonitis, myocardial infarction, neuropathy, petechiae, pruritus, pulmonary edema, pulmonary fibrosis, radiation recall phenomenon, renal failure, respiratory failure, reversible posterior leukoencephalopathy syndrome, sepsis, supraventricular cardiac arrhythmia, thrombotic thrombocytopenic purpura.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Please report any adverse drug reactions via contacting Cedal Nano.
OVERDOSAGE:
There is no known antidote for overdose of gemcitabine. Doses as high as 5700 mg/m2 have been administered by intravenous infusion over 30-minutes every 2 weeks with clinically acceptable toxicity. In the event of suspected overdose, the patient should be monitored with appropriate blood counts and receive supportive therapy, as necessary.
Drug Interactions
The most important drug interactions of Gemcitabine involve its use in combination with other chemotherapeutic agents and supportive treatments, where the risk of toxicity may increase. When used with cisplatin, Gemcitabine can lead to enhanced myelosuppression and nephrotoxicity, requiring close monitoring of renal function and blood counts. In combination with paclitaxel, particularly when paclitaxel is administered first, there is a higher risk of neutropenia and peripheral neuropathy, making the sequence of administration critical. Gemcitabine also acts as a radiosensitizer, so concurrent or closely timed radiotherapy may result in severe pulmonary or gastrointestinal toxicity. Additionally, due to its immunosuppressive effects, the use of live vaccines during or shortly after treatment is contraindicated, as it may increase the risk of serious infections. These interactions highlight the need for careful scheduling, monitoring, and clinical judgment when Gemcitabine is used in multi-modality cancer treatment.
Use in pregnancy and lactation
- Pregnancy
There are no adequate data from the use of gemcitabine in pregnant women. Studies in animals have shown reproductive toxicity. Based on results from animal studies and the mechanism of action of gemcitabine, this substance should not be used during pregnancy unless clearly necessary. Women should be advised not to become pregnant during treatment with gemcitabine and to warn their attending physician immediately, should this occur after all.
- Breastfeeding
It is not known whether gemcitabine is excreted in human milk and adverse effects on the suckling child cannot be excluded. Breast-feeding must be discontinued during gemcitabine therapy.
- Fertility
In fertility studies, gemcitabine caused hypospermatogenesis in male mice. Therefore, men undergoing treatment with gemcitabine are advised not to father a child during treatment and for up to six months after its completion. Due to the potential risk of infertility associated with gemcitabine therapy, patients should seek medical advice regarding sperm cryopreservation prior to the start of treatment.
- Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. However, gemcitabine has been reported to cause mild to moderate somnolence, especially in combination with alcohol consumption. Patients should be cautioned against driving or operating machinery until it is established that they do not become somnolent.
Storage Conditions
Gemcedal® is supplied as vials containing gemcitabine 200 mg, 1000 mg as Concentrate for Solution for Infusion.
- Keep the medicine in the box until it is consumed.
- Store in a refrigerator (2°C-8°C).
- Store away from light and moisture.
- Keep the medicine out of the reach of children.
- The normal safety precautions for cytostatic agents must be observed when preparing and disposing of the infusion solution. Handling of the concentrate should be done in a safety box and protective coats and gloves should be used. If no safety box is available, the equipment should be supplemented with a mask and protective glasses.
- If the preparation comes into contact with the eyes, this may cause serious irritation. The eyes should be rinsed immediately and thoroughly with water. If there is lasting irritation, a doctor should be consulted. If the solution is spilled on the skin, rinse thoroughly with water.
- Nature and contents of container
- 200 mg/5.3 ml presentation
- Each vial of the 200mg presentation contains 5.3ml concentrate. Each pack contains 1 vial.
- 1 g/26.3 ml presentation
- Each vial of the 1g presentation contains 26.3ml concentrate. Each pack contains 1 vial.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.