IFOCEDAL® injection is an alkylating drug indicated for use in combination with certain other approved antineoplastic agents for third-line chemotherapy of germ cell testicular cancer. It should be used in combination with mesna for prophylaxis of hemorrhagic cystitis. The drug also has been designated an orphan drug by FDA for use in the treatment of various bone and soft tissue sarcomas and usually is included as a component of various regimens for initial chemotherapy in these sarcomas. In addition, ifosfamide is used for initial or second- or third-line therapy in the treatment of various other malignancies including lung cancer, cervical cancer and ovarian cancer.
IfoCedal®
Generic Name
Brand Name
Drug Class
Dosage Form
Indications
Contradications
Warnings and Precautions
Dosage and administration
Adverse Reactions
Drug Interactions
Pregnancy and Lactation
Storage Conditions
Indications
Contradications
Ifosfamide is contraindicated in patients with:
- Known hypersensitivity to administration of ifosfamide.
- Urinary outflow obstruction.
Warnings and Precautions
Myelosuppression, Immunosuppression, and Infections
Treatment with ifosfamide may cause myelosuppression and significant suppression of
immune responses, which can lead to severe infections. Fatal outcomes of ifosfamide-associated myelosuppression have been reported. Ifosfamide-induced myelosuppression can cause leukopenia, neutropenia, thrombocytopenia (associated with a higher risk of bleeding events), and anemia. The nadir of the leukocyte count tends to be reached approximately during the second week after administration. When ifosfamide is given in combination with other chemotherapeutic/hematotoxic agents and/or radiation therapy, severe myelosuppression is frequently observed. The risk of myelosuppression is dose-dependent and is increased with administration of a single high dose compared with fractionated administration. The risk of myelosuppression is also increased in patients with reduced renal function.
Severe immunosuppression has led to serious, sometimes fatal, infections. Sepsis and
septic shock also have been reported. Infections reported with ifosfamide include pneumonias, as well as other bacterial, fungal, viral, and parasitic infections. Latent infections can be reactivated. In patients treated with ifosfamide, reactivation has been reported for various viral infections. Infections must be treated appropriately. Antimicrobial prophylaxis may be indicated in certain cases of neutropenia at the discretion of the managing physician. In case of neutropenic fever, antibiotics and/or antimycotics must be given. Close hematologic monitoring is recommended. White blood cell (WBC) count, platelet count and hemoglobin should be obtained prior to each
administration and at appropriate intervals after administration. Unless clinically essential,
ifosfamide should not be given to patients with a WBC count below 2000/μL and/or a platelet count below 50,000/μL.
Ifosfamide should be given cautiously, if at all, to patients with presence of an infection, severe immunosuppression or compromised bone marrow reserve, as indicated by leukopenia, granulocytopenia, extensive bone marrow metastases, prior radiation therapy, or prior therapy with other cytotoxic agents.
Central Nervous System Toxicity, Neurotoxicity
Administration of ifosfamide can cause CNS toxicity and other neurotoxic effects. The
risk of CNS toxicity and other neurotoxic effects necessitates careful monitoring of the
patient. Neurologic manifestations consisting of somnolence, confusion, hallucinations,
blurred vision, psychotic behavior, extrapyramidal symptoms, urinary incontinence,
seizures, and in some instances, coma, have been reported following ifosfamide
therapy. There have also been reports of peripheral neuropathy associated with
ifosfamide use.
Ifosfamide neurotoxicity may manifest within a few hours to a few days after first
administration and in most cases resolves within 48 to 72 hours of ifosfamide
discontinuation. Symptoms may persist for longer periods of time. Supportive therapy
should be maintained until their complete resolution. Occasionally, recovery has been
incomplete. Fatal outcomes of CNS toxicity have been reported. Recurrence of CNS
toxicity after several uneventful treatment courses has been reported. If encephalopathy develops, administration of ifosfamide should be discontinued.
Due to the potential for additive effects, drugs acting on the CNS (such as antiemetics,
sedatives, narcotics, or antihistamines) must be used with particular caution or, if
necessary, be discontinued in case of ifosfamide-induced encephalopathy.
Manifestations of CNS toxicity may impair a patient’s ability to operate an automobile or
other heavy machinery.
Renal and Urothelial Toxicity and Effects
Ifosfamide is both nephrotoxic and urotoxic. Glomerular and tubular kidney function
must be evaluated before commencement of therapy as well as during and after treatment. Monitor urinary sediment regularly for the presence of erythrocytes and other signs of uro/nephrotoxicity. Monitor serum and urine chemistries, including phosphorus and potassium regularly. Administer appropriate replacement therapy as indicated. Renal parenchymal and tubular necrosis have been reported in patients treated with ifosfamide. Acute tubular necrosis, acute renal failure, and chronic renal failure secondary to ifosfamide therapy have been reported, and fatal outcome from nephrotoxicity has been documented.
Disorders of renal function, (glomerular and tubular) following ifosfamide administration
are very common. Manifestations include a decrease in glomerular filtration rate, increased serum creatinine, proteinuria, enzymuria, cylindruria, aminoaciduria, phosphaturia, and glycosuria as well as tubular acidosis. Fanconi syndrome, renal rickets, and growth retardation in children as well as osteomalacia in adults also have been reported. Development of a syndrome resembling SIADH (syndrome of inappropriate antidiuretic hormone secretion) has been reported with ifosfamide.
Tubular damage may become apparent during therapy, months or even years after cessation of treatment. Glomerular or tubular dysfunction may resolve with time, remain stable, or progress over a period of months or years, even after completion of ifosfamide treatment.
The risk and expected benefits of ifosfamide therapy should be carefully weighed when
considering the use of ifosfamide in patients with preexisting renal impairment or reduced nephron reserve.
Urotoxic side effects, especially hemorrhagic cystitis, have been very commonly associated with the use of ifosfamide. These urotoxic effects can be reduced by prophylactic use of mesna.
Hemorrhagic cystitis requiring blood transfusion has been reported with ifosfamide. The risk of hemorrhagic cystitis is dose-dependent and increased with administration of single high doses compared to fractionated administration. Hemorrhagic cystitis after a single dose of ifosfamide has been reported. Past or concomitant radiation of the bladder or busulfan treatment may increase the risk for hemorrhagic cystitis.
Before starting treatment, it is necessary to exclude or correct any urinary tract
obstructions.
During or immediately after administration, adequate amounts of fluid should be ingested or infused to force dieresis in order to reduce the risk of urinary tract toxicity.
Obtain a urinalysis prior to each dose of ifosfamide. If microscopic hematuria (greater than 10 RBCs per high power field) is present, then subsequent administration should be withheld until complete resolution. Further administration of ifosfamide should be given with vigorous oral or parenteral hydration.
Ifosfamide should be used with caution, if at all, in patients with active urinary tract infections.
Cardiotoxicity
Manifestations of cardiotoxicity reported with ifosfamide treatment include:
– Supraventricular or ventricular arrhythmias, including atrial/supraventricular tachycardia, atrial fibrillation, pulseless ventricular tachycardia
– Decreased QRS voltage and ST-segment or T-wave changes
– Toxic cardiomyopathy leading to heart failure with congestion and hypotension
– Pericardial effusion, fibrinous pericarditis, and epicardial fibrosis
Fatal outcome of ifosfamide-associated cardiotoxicity has been reported.
The risk of developing cardiotoxic effects is dose-dependent. It is increased in patients with prior or concomitant treatment with other cardiotoxic agents or radiation of the cardiac region and, possibly, renal impairment.
Particular caution should be exercised when ifosfamide is used in patients with risk
factors for cardiotoxicity and in patients with preexisting cardiac disease.
Pulmonary Toxicity
Interstitial pneumonitis, pulmonary fibrosis, and other forms of pulmonary toxicity have been reported with ifosfamide treatment. Pulmonary toxicity leading to respiratory failure as well as fatal outcome has also been reported. Monitor for signs and symptoms of pulmonary toxicity and treat as clinically indicated.
Secondary Malignancies
Treatment with ifosfamide involves the risk of secondary tumors and their precursors as
late sequelae. The risk of myelodysplastic alterations, some progressing to acute leukemias, is increased. Other malignancies reported after use of ifosfamide or regimens with ifosfamide include lymphoma, thyroid cancer, and sarcomas.
The secondary malignancy may develop several years after chemotherapy has been discontinued.
Veno-occlusive Liver Disease
Veno-occlusive liver disease has been reported with chemotherapy that included ifosfamide.
Effects on Fertility
Ifosfamide interferes with oogenesis and spermatogenesis. Amenorrhea, azoospermia, and sterility in both sexes have been reported. Development of sterility appears to depend on the dose of ifosfamide, duration of therapy, and state of gonadal function at the time of treatment. Sterility may be irreversible in some patients.
Female Patients
Amenorrhea has been reported in patients treated with ifosfamide. The risk of permanent chemotherapy-induced amenorrhea increases with age. Pediatric patients treated with ifosfamide during prepubescence subsequently may not conceive and those who retain ovarian function after completing treatment are at increased risk of developing premature menopause.
Male Patients
Men treated with ifosfamide may develop oligospermia or azoospermia. Pediatric patients treated with ifosfamide during prepubescence might not develop secondary sexual characteristics normally, but may have oligospermia or azoospermia. Azoospermia may be reversible in some patients, though the reversibility may not occur for several years after cessation of therapy. Sexual function and libido are generally unimpaired in these patients. Some degree of testicular atrophy may occur. Patients treated with ifosfamide have subsequently fathered children.
Anaphylactic/Anaphylactoid Reactions and Cross-sensitivity
Anaphylactic/anaphylactoid reactions have been reported in association with ifosfamide. Cross sensitivity between oxazaphosphorine cytotoxic agents has been reported.
Impairment of Wound Healing
Ifosfamide may interfere with normal wound healing.
Dosage and administration
Dosage:
Ifosfamide Injection should be administered intravenously at a dose of 1.2 grams per m2 per day for 5 consecutive days. Treatment is repeated every 3 weeks or after recovery from hematologic toxicity.
In order to prevent bladder toxicity, ifosfamide injection should be given with extensive hydration consisting of at least 2 liters of oral or intravenous fluid per day. Mesna should be used to reduce the incidence of hemorrhagic cystitis. Ifosfamide injection should be administered as a slow intravenous infusion lasting a minimum of 30 minutes.
Method of Administration:
IFOCEDAL® is administered by IV infusion. IV infusions of IFOCEDAL® should be administered over a period of at least 30 minutes; the drug also has been administered by continuous IV infusion.
To minimize urotoxicity, patients should be adequately hydrated prior to and during IFOCEDAL® therapy (e.g., 2 liters of oral or IV fluid daily). In addition, a uroprotective agent such mesna should be administered during IFOCEDAL® therapy to decrease the incidence of ifosfamide-induced bladder toxicity (e.g., hemorrhagic cystitis, hematuria); adequate uroprotection is particularly important at relatively high dosages.
Solutions of IFOCEDAL® injection may be diluted further to achieve concentrations of 0.6 to 20 mg/mL in the following fluids:
5% Dextrose Injection
0.9% Sodium Chloride Injection
Lactated Ringer’s Injections
Sterile Water for Injection
Because essentially identical stability results were obtained for Sterile Water admixtures
as for the other admixtures (5% Dextrose Injection, 0.9% Sodium Chloride Injection, and
Lactated Ringer’s Injection), the use of large volume parenteral glass bottles, Viaflex
bags or PAB™ bags that contain intermediate concentrations or mixtures of excipients
(e.g., 2.5% Dextrose Injection, 0.45% Sodium Chloride Injection, or 5% Dextrose and
0.9% Sodium Chloride Injection) is also acceptable.
Further diluted solutions of IFOCEDAL® injection should be refrigerated and used within
24 hours.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Adverse Reactions
Like all medicines, this medicine can cause side effects, although not everybody gets them. Side effects with IFOCEDAL® may include:
- >10%:
Central nervous system: Brain disease (≤15%), central nervous system toxicity (≤15%)
Dermatologic: Alopecia (83% to 90%; combination therapy: 100%)
Endocrine & metabolic: Metabolic acidosis (31%)
Gastrointestinal: Nausea (≤58%), vomiting (≤58%)
Hematologic & oncologic: Leukopenia (≤100%; grade 4: ≤50%; nadir: 8 to 14 days), anemia (38%), thrombocytopenia (20%; grades 3/4: ≤8%)
Renal: Hematuria (6% to 92%, reduced with mesna; grade 2 [gross hematuria]: 8% to 12%)
- 1-10%:
Cardiovascular: Localized phlebitis (2% to 3%)
Gastrointestinal: Anorexia (1%)
Hematologic & oncologic: Febrile neutropenia (1%)
Hepatic: Hepatic insufficiency (2% to 3%), increased serum bilirubin (2% to 3%), increased serum transaminases (2% to 3%)
Infection: Infection (8% to 10%)
Renal: Renal insufficiency (6%)
Miscellaneous: Fever (1%)
- <1%:
Postmarketing, and/or case reports: Abdominal pain, abnormal gait, acute renal failure, agranulocytosis, altered hormone level (increased gonadotropin), amenorrhea, amnesia, anaphylaxis, angina pectoris, angioedema, anovulation, anuria, arthralgia, asterixis, atrial premature contractions, atrial fibrillation, atrial flutter, atrial premature contractions, azoospermia, blood coagulation disorder, blurred vision, bone marrow failure, bradycardia, bradyphrenia, bronchospasm, bundle branch block, capillary leak syndrome, cardiac arrhythmia, cardiac failure, cardiogenic shock, cardiomyopathy, cardiotoxicity, casts in urine, catatonia, chest pain, chills, cholestasis, chronic renal failure, colitis, conjunctivitis, constipation, cough, increased serum creatinine, decreased creatinine clearance, decreased plasma estrogen concentration, deep vein thrombosis, delirium, delusions, dermatitis, diarrhea, disseminated intravascular coagulation, dysarthria, dysesthesia, dyspnea, dysuria, ECG abnormality (QRS complex abnormal), edema, enterocolitis, erythema, extrapyramidal reaction, facial swelling, Fanconi’s syndrome, fatigue, fecal incontinence, flushing, fulminant hepatitis, gastrointestinal hemorrhage, glycosuria, granulocytopenia, growth suppression (children), hearing loss, hemolytic anemia, hemolytic-uremic syndrome, hemorrhage (including myocardial), hemorrhagic cystitis, hepatic failure, hepatic sinusoidal obstruction syndrome (formerly known as hepatic veno-occlusive disease), hepatitis (cytolytic), hepatorenal syndrome, herpes zoster, hyperglycemia, hyperhidrosis, hypertension, hyperpigmentation, hypersensitivity pneumonitis, hypersensitivity reaction, hypocalcemia, hypoesthesia, hypokalemia, hyponatremia, hypophosphatemia, hypotension, hypoxia, intestinal obstruction, immunosuppression, increased blood urea nitrogen, increased creatinine clearance, increased gamma-glutamyl transferase, increased lactate dehydrogenase, increased serum alkaline phosphatase, infertility, infusion site reaction (erythema, inflammation, pain, pruritus, swelling, tenderness), inhibition of spermatogenesis, interstitial nephritis, interstitial pneumonitis, interstitial pulmonary disease, inversion T wave on ECG, irritable bladder, jaundice, left ventricular dysfunction (failure), leukoencephalopathy, limb pain, lymphocytopenia, malaise, mania, menopause (premature), mental status changes, metastases (including ALL, AML, APL, lymphoma, MDS, RCC, sarcomas, thyroid cancer), methemoglobinemia, mucosal inflammation, mucous membrane ulceration, multi-organ failure, muscle twitching, mutism, myalgia, myocardial infarction, myocarditis, nail disease, nephrogenic diabetes insipidus, neuralgia, neutropenia, oligospermia, oliguria, osteomalacia (adults), ovarian failure, pain, palmar-plantar erythrodysesthesia, pancreatitis, pancytopenia, panic attack, paranoia, parenchymal damage (renal), paresthesia, pericardial effusion, pericarditis, peripheral neuropathy, petechia, phosphaturia, physical health deterioration, pleural effusion, pneumonia (including Pneumocystis jirovecii), pneumonitis, pollakiuria, polydipsia, polyneuropathy, polyuria, portal vein thrombosis, progressive multifocal leukoencephalopathy, proteinuria, pruritus, pulmonary edema, pulmonary embolism, pulmonary fibrosis, pulmonary hypertension, reduced ejection fraction, renal tubular acidosis, renal tubular necrosis, respiratory distress syndrome (acute), respiratory failure, reversible posterior leukoencephalopathy syndrome, rhabdomyolysis, rickets, salivation, seizure, sepsis, septic shock, SIADH, skin abnormalities related to radiation recall, skin necrosis, skin rash (including macular and papular), status epilepticus, sterility, Stevens-Johnson syndrome, stomatitis, ST segment changes on ECG, supraventricular extrasystole, tachycardia, talkativeness (logorrhea), tinnitus, toxic epidermal necrolysis, tumor lysis syndrome, typhlitis, uremia, urinary incontinence, urine abnormality (aminoaciduria and enzymuria), urticaria, vasculitis, ventricular fibrillation, ventricular premature contractions, ventricular tachycardia, vertigo, viral hepatitis, visual impairment, wound healing impairment
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Please report any adverse drug reactions via contacting Cedal Nano.
Overdosage
No specific antidote for ifosfamide is known. Patients who receive an overdose should be closely monitored for the development of toxicities. Serious consequences of overdosage include manifestations of dose-dependent toxicities such as CNS toxicity, nephrotoxicity, myelosuppression, and mucositis. Management of overdosage would include general supportive measures to sustain the patient through any period of toxicity that might occur, including appropriate state-of-the-art treatment for any concurrent infection, myelosuppression, or other toxicity. Ifosfamide as well as ifosfamide metabolites are dialyzable.
Cystitis prophylaxis with mesna may be helpful in preventing or limiting urotoxic effects
with overdose. Methylene blue has been used in the management of ifosfamide-induced encephalopathy.
Drug Interactions
Ifosfamide is a substrate for both CYP3A4 and CYP2B6.
Inducers of CYP3A4
CYP3A4 inducers (e.g., carbamazepine, phenytoin, fosphenytoin, phenobarbital, rifampin, St. John Wort) may increase the metabolism of ifosfamide to its active alkylating metabolites. CYP3A4 inducers may increase the formation of the neurotoxic/nephrotoxic ifosfamide metabolite, chloroacetaldehyde. Closely monitor patients taking ifosfamide with CYP3A4 inducers for toxicities and consider dose adjustment.
Inhibitors of CYP3A4
CYP3A4 inhibitors (e.g., ketoconazole, fluconazole, itraconazole, sorafenib, aprepitant, fosaprepitant, grapefruit, grapefruit juice) may decrease the metabolism of ifosfamide to its active alkylating metabolites, perhaps decreasing the effectiveness of ifosfamide treatment.
Pregnancy and Lactation
Use in Pregnancy
Ifosfamide can cause fetal harm when administered to a pregnant woman. Fetal growth retardation and neonatal anemia have been reported following exposure to ifosfamide-containing chemotherapy regimens during pregnancy. Ifosfamide is genotoxic and mutagenic in male and female germ cells. Embryotoxic and teratogenic effects have been observed in mice, rats and rabbits at doses 0.05 to 0.075 times the human dose. Women should not become pregnant and men should not father a child during therapy with ifosfamide. Further, men should not father a child for up to 6 months after the end of therapy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug or after treatment, the patient should be apprised of the potential hazard to a fetus.
Use in Breast feeding
Ifosfamide is distributed into milk. Because of the potential for serious adverse reactions to ifosfamide in nursing infants, a decision should be made whether to discontinue nursing or the drug, taking into account the importance of the drug to the woman.
Pediatric use
Safety and effectiveness have not been established in pediatric patients.
Geriatric use
In general, dose selection for an elderly patient should be cautious, reflecting the
greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. A study of patients 40 to 71 years of age indicated that elimination half-life appears to increase with advancing age. This apparent increase in
half-life appeared to be related to increases in volume of distribution of ifosfamide with
age. No significant changes in total plasma clearance or renal or non-renal clearance with age were reported. Ifosfamide and its metabolites are known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Use in patients with renal impairment
No formal studies were conducted in patients with renal impairment. Ifosfamide and its
metabolites are known to be excreted by the kidneys and may accumulate in plasma
with decreased renal function. Patients with renal impairment should be closely
monitored for toxicity and dose reduction may be considered. Ifosfamide and its
metabolites are dialyzable.
Use in patients with hepatic impairment
No formal studies were conducted in patients with hepatic impairment. Ifosfamide is
extensively metabolized in the liver and forms both efficacious and toxic metabolites.
Ifosfamide should be given cautiously to patients with impaired hepatic function.
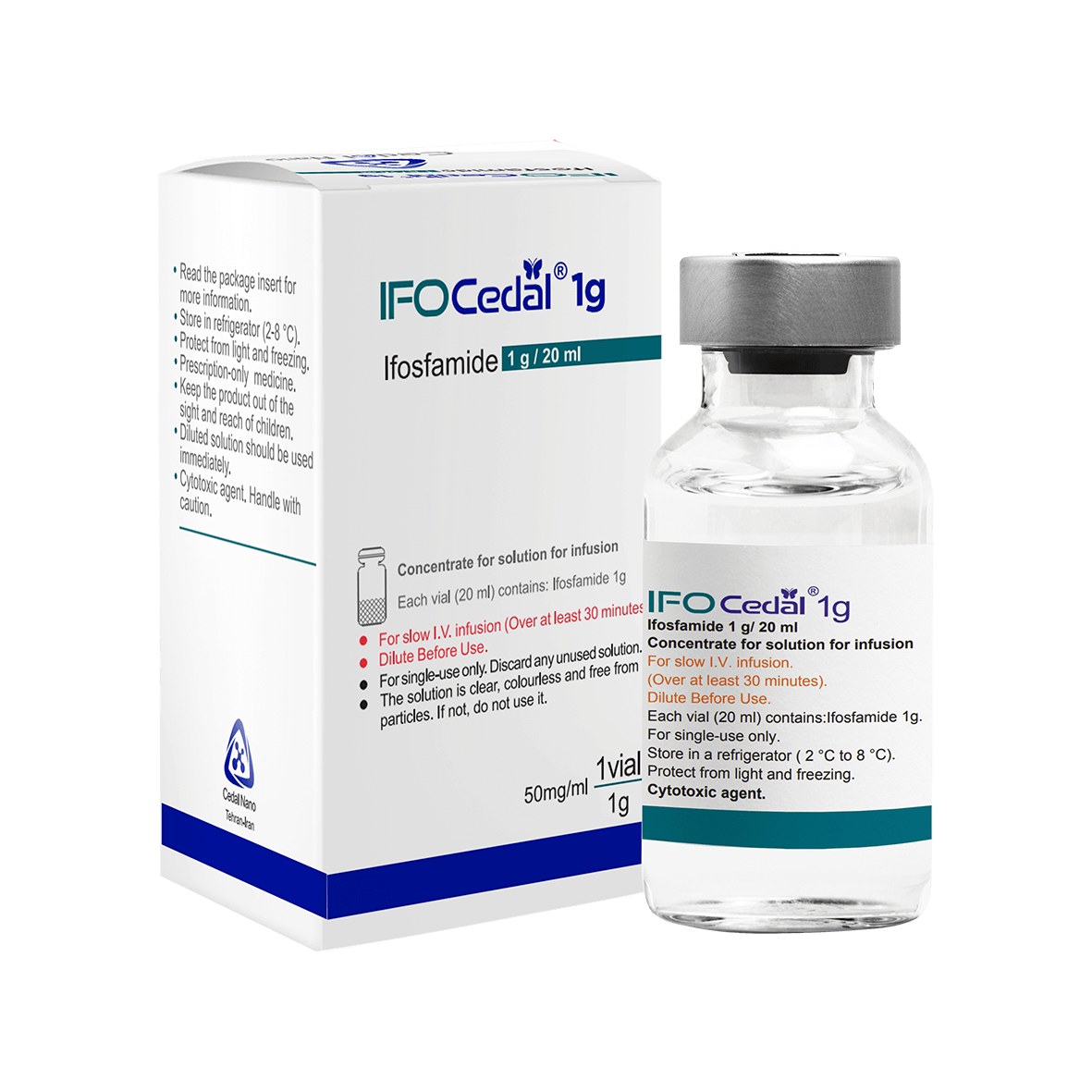
Storage Conditions
Store IFOCEDAL® concentrate for solution for infusion in refrigerator (2-8 °C). Protect from freezing.
Store in original package in order to protect from light.
IFOCEDAL® is supplied as vials containing Ifosfamide equivalent to 1 g and 2 g as concentrate for solution for infusion.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Because of the carcinogenic potential of ifosfamide, the usual precautions for handling and preparing solutions of cytotoxic drugs should be observed. The manufacturer recommends use of protective gloves when handling ifosfamide since accidental exposure may be associated with skin reactions. If ifosfamide solution comes in contact with skin or mucosa, affected skin areas should be washed immediately and thoroughly with soap and water and affected mucosa should be thoroughly rinsed with copious amounts of water.
From a microbiological point of view, the product should be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would not normally be longer than 8 hours at 2-8 °C.